The Journey of Imperfection
How can the telemedical field in British Columbia be improved to better serve people suffering from skin problems, while also providing the tools to empower people to combat their challenges and de-stigmatize imperfections? Let me explain.

Process
Ideating, Empathizing, User Testing, Strategizing, Prototyping
Duration
10 Weeks
Tools
Figma, Invision, Sketch, POP by Marvel
PROBLEM SPACE ONE
Clear lack of dermatologists in BC with a doctor-to-patient ratio of 1 Dermatologist per 78,015 patients.
SOLUTION
Create an easy to use and accessible solution to users who don't have access to a dermatologist. By doing so, we provide the care they need to move along their skin journey.
PROBLEM SPACE TWO
Post-patient care is nonexistent. Patients are handed a prescription with no understanding of how it works.
SOLUTION
Add a place for users to go to for resources on ingredients, and recommended products that they can use based on the dermatologist's diagnosis.
Introduction
From a personal stance, I have always had problems with my skin. Dealing with dozens of products that are deemed to help acne-prone skin which resulted in nothing, along with doctors that treated me like “Patient 524” rather than Alex, I’ve had to learn my skin through trial-and-error (and money), rather than sorting it out with professional help from the start.
There are many challenges with dealing with skin problems: Who do you talk to? What do I actually have? What can I use to help? All these are typical questions from people suffering from skin concerns, but sadly are much more than just surface level. Skin concerns can not only affect the physical appearance of people, but often can cause significant psychological stress as well. While the notion of “everyone is beautiful” is absolutely true, having a face that needs a mere splash of water to look fresh is an ideal that doesn’t sound too bad. The pursuit for faultless skin is a beauty standard in every culture, but why does it vary so much?
I chose to focus on British Columbia’s system and culture as it’s the one I’m most familiar with, and found some eye-opening details that are disheartening. My goal with this Case Study was to find a way to help people navigate their way through the emotional and physical struggle of a skin journey, so they wouldn’t have to suffer as long as I did. The Journey of Imperfection is just that, a journey that isn’t always perfect, but leads to progress that can be looked back on and be acknowledged as progress in the right direction. Just like good design, the road isn’t always direct and wrong turns will be made, but you’ll always end up at the end.
Problem Space
While dealing with my personal concerns, I tried nearly every avenue of resources without much success. Family doctors weren’t necessarily equipped to answer skin-related questions, dermatologists were incredibly hard to see from the complete lack of them in British Columbia, and websites/YouTube were fairly unreliable. Because of this, I wanted to focus on a few tangential problem spaces.
The first of which was tackling the lack of dermatologists in BC. While it’s clear that they don’t grow on trees, the method of booking and visiting dermatologists can be drastically improved. With the sudden appearance of COVID-19, the healthcare field needed to shift to online models, thus the rise of tele-medical appointments occurred. In BC, these were instantly brilliant - having the ability to see a General Practitioner within an hour covered under BC’s MSP plan was truly remarkable.
The only issue lies in the fact that dermatologists were not included in the coverage, costing around $180 for a single appointment. This brings a dilemma to people: wait for months to get an appointment for free, or pay to get an appointment immediately? Why not both, I pondered. The rapid speed of a tele-medical appointment with the flexibility of MSP coverage would be a match like Sonny & Cher.
PROBLEM SPACE ONE
Lack of dermatologists in BC with a doctor-to-patient ratio of one dermatologist per 78,015 people
PROBLEM SPACE TWO
Post-patient care is poor. Patients are handed only a prescription with no real understanding of how it works
The second issue revolves around the post-care process, specifically receiving a prescription. As we are all familiar, a Rx note comes with vague symbols that are supposed to represent the English language, and on it are basic things to help the pharmacist get what you need.
The issue here is that this information helps the pharmacist, not you. Receiving a prescription for eczema? You know the name of it, sure, and perhaps the dose and when and/or where to use it, but do you know what it can be used with? Does it fit with your current routine? Do the products you’re currently using make it worse? Better? We don’t know, and that’s an issue.
I’d like to help people understand their prescriptions better. Given a new product, how does it interact with what they’re currently using? I found it challenging to find this out on my own, so I can only imagine how lost some may feel when they have no control or autonomy trying to face these skin concerns.
Project Constraints
There are admittedly some constraints with a problem space such as the following. Some are policy related (adding Dermatology to MSP tele-medical coverage) but also socially related (remove the stigma towards imperfect skin, and the condescension from others when wanting to seek help). With this in mind, tackling such an issue will have roadblocks, but if it can help one person feel a little bit better about themselves, I can rest easy at night.
Regarding the project as a whole, only having 10 weeks was a limited window to research and develop was challenging, but I believe I have built something that can help someone.
How Might We
How might we support patients with skin concerns from the booking experience to product recommendations in order to improve the pre-existing medical system while providing necessary post-appointment care and resources?
Current Medical System
As I briefly mentioned, the problems I’m focusing on are in the BC medical system, simply because it’s the one I’m most familiar with and can find the most research on. If I were a BC resident and looking to book a dermatology appointment, I would do the following: first, I would book an appointment to see my doctor (at this stage, either in-person or via a tele-medical app would work), then would be referred to a dermatologist in my area.
This “referral” is the red flag in this situation, since the average wait time for a dermatologist in BC is around 7 months (BC Children’s Hospital) and can be even longer for less urgent cases. 7 months is a considerable amount of time for someone who is looking in the mirror every morning, covering up blemishes and scars before they go out, and dealing with the burden of just waiting for help.
The indirect issue with this process is that it doesn’t represent a significant amount of BC’s population. The current dermatologist-to-patient ratio is 1:78,015 - alarming, I know. Even worse still, that ratio is averaged for the population as a whole, and doesn’t account for the fact that a significant amount of dermatologists (65, as of 2015) live either on Vancouver Island or in Metro Vancouver. Those living in northern or remote areas of BC simply do not have access to in-person appointments.
Key Insights from User Interviews
Interviews were difficult to conduct for this project, I can’t sugarcoat that fact. Going into the process, I imagined having a pool of people that have long struggled with skin concerns... that wasn’t the case. My criteria for seeking out participants to interview was fairly simple: be a resident of BC, and had recently visited a dermatologist. Alas it was not simple, I believe the lack of available participants highlights the inherently broken system of BC’s medical process. I had managed to find 2 participants - this is what I discovered:
Wait times
Among interviewees and secondary research, the wait times for these appointments is far too long. Patients have elevated stress levels during those periods, and can potentially worsen their condition with the prolonged wait.
Lack of information
The general practitioners seem to lack fairly straightforward skin-related questions patients may have, and will tend to prescribe products using a shotgun approach, rather than targeted care. Furthermore, once the dermatologist is seen, the patients are not provided any information other than “Trust me, I’m a Doctor”, leading to reduced rates of confidence in the process. From the interviews, it was learned that the problems both interviewees had were solved without much help from specialists, rather their own research and experimentation.
Lack of Urgency
Doctors seem to overlook the stress skin concerns can have on patients, and will often delay referrals to specialists even though they don’t understand the scope of the problem, and would be in the patients best interest to refer them as quickly as possible.
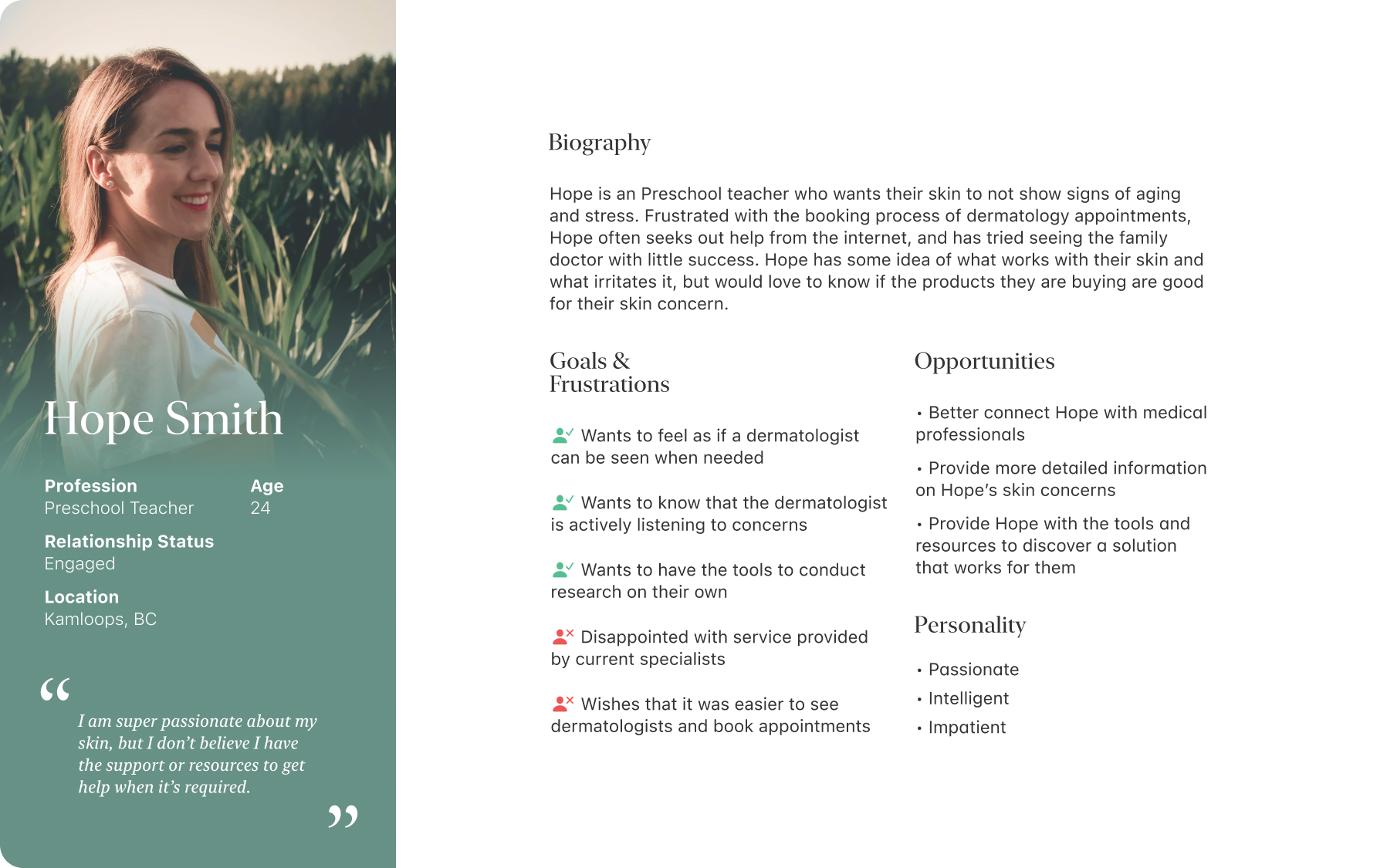
Persona
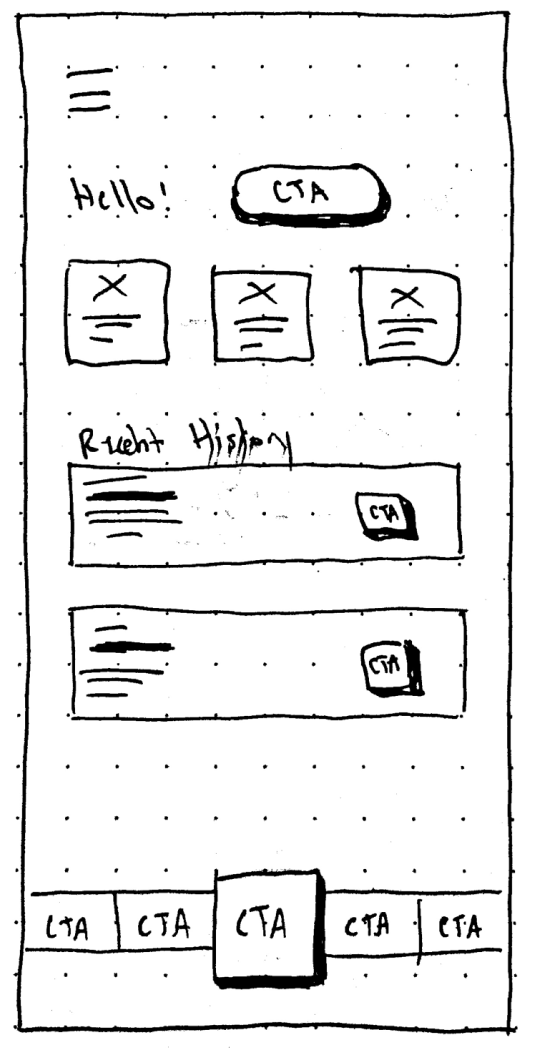
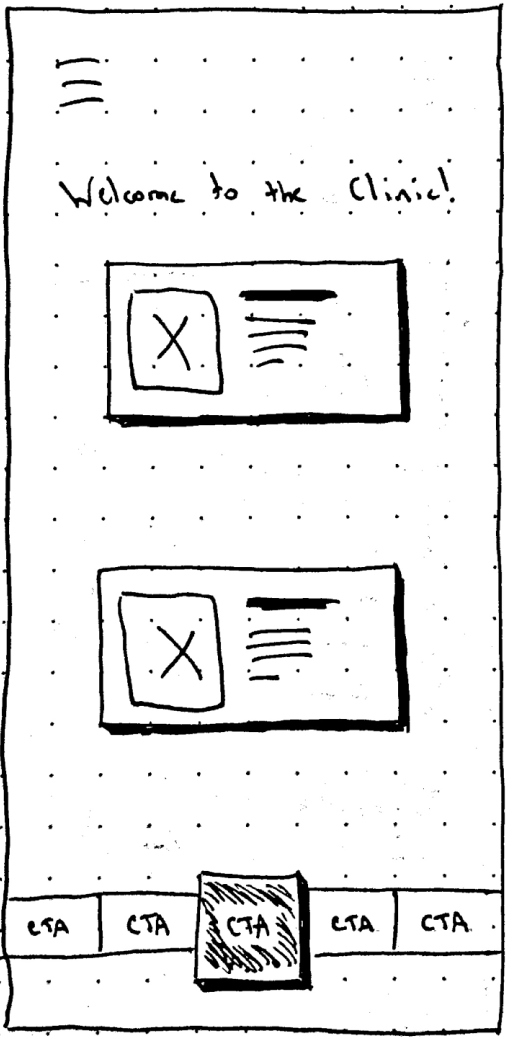
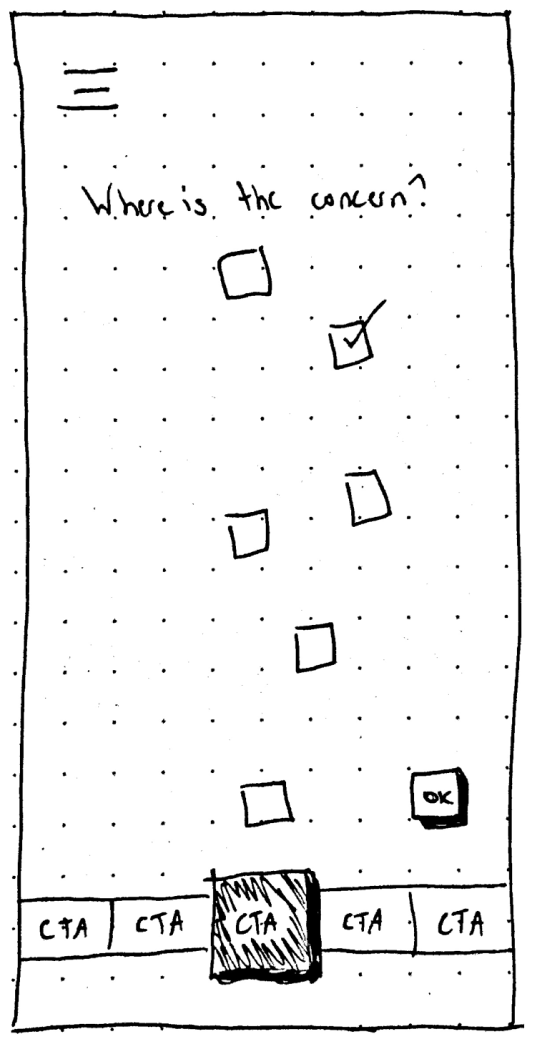
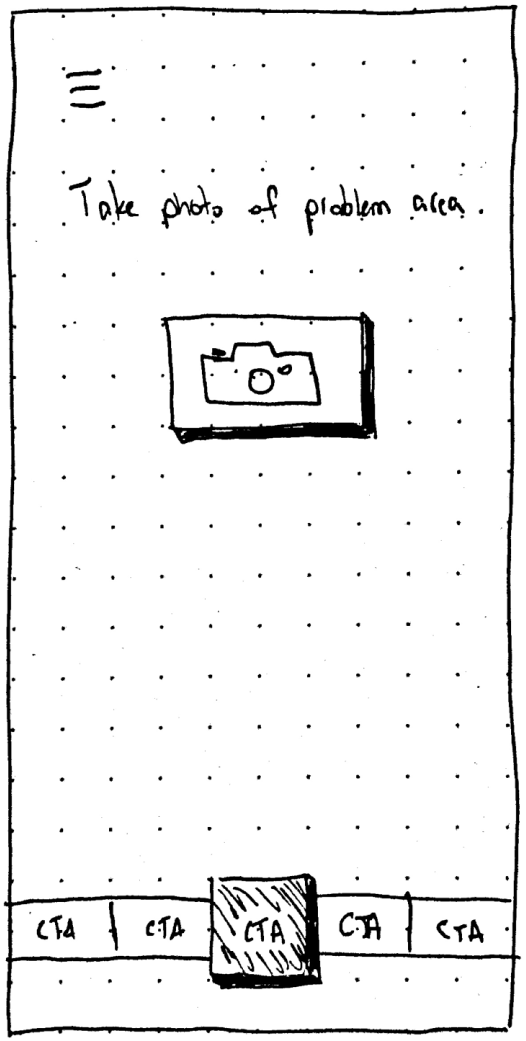
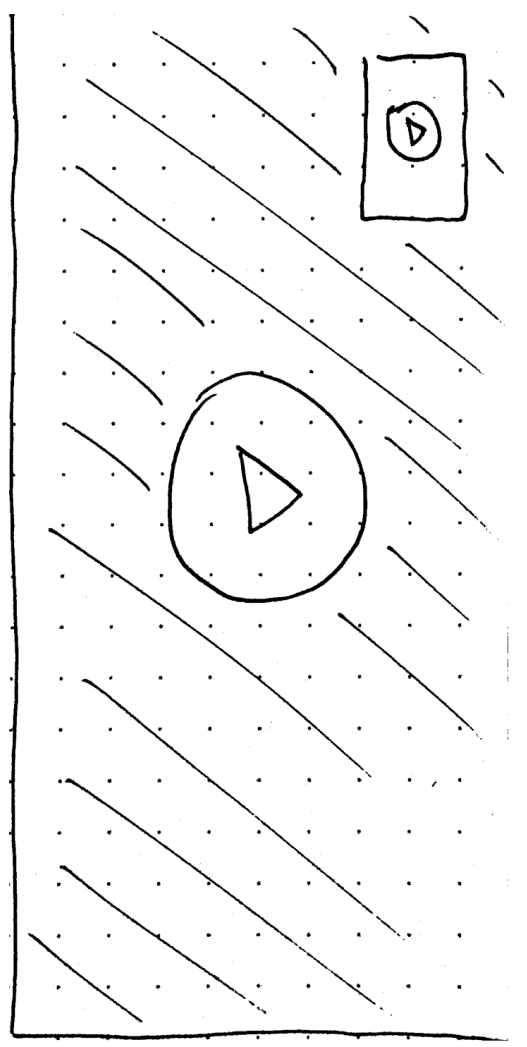
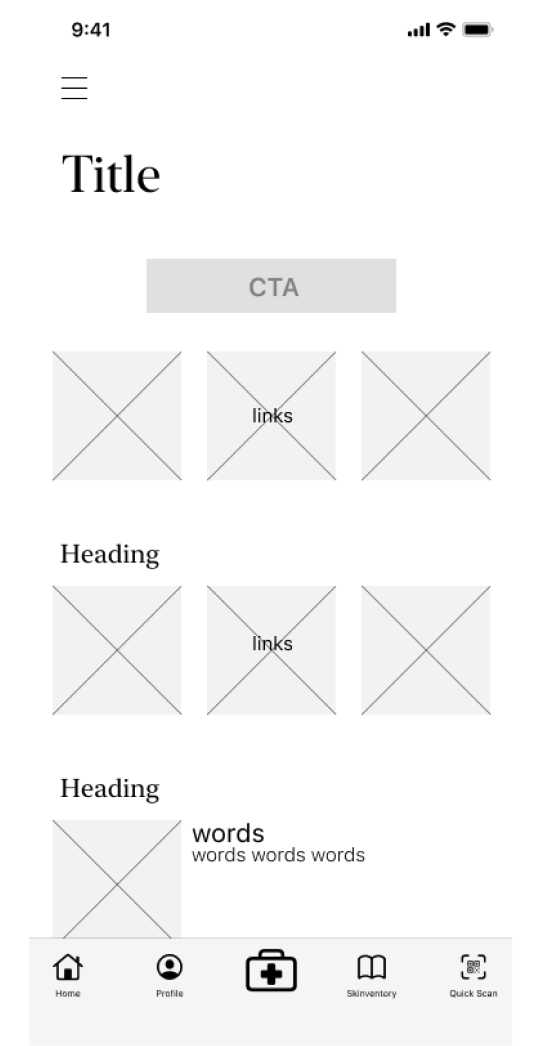
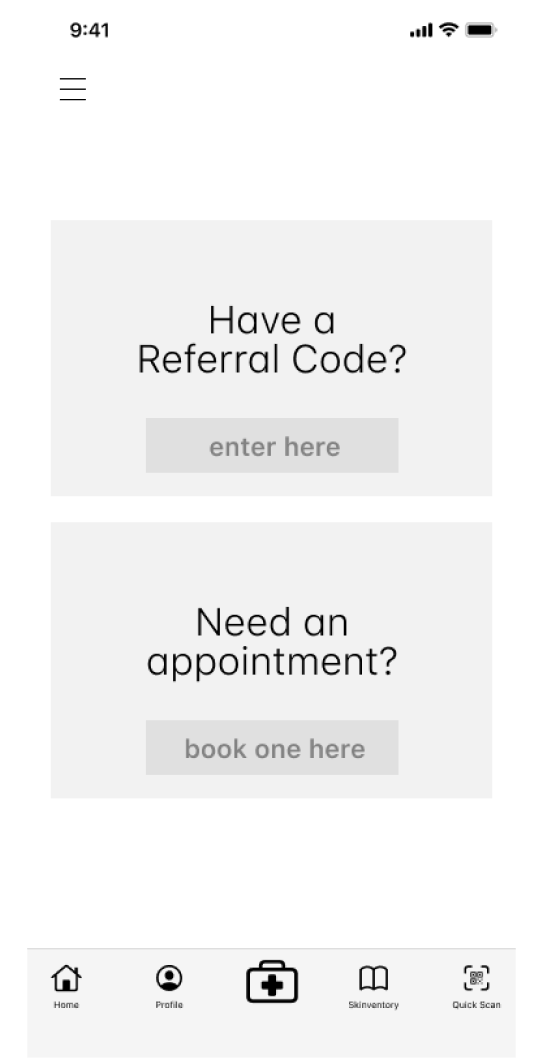
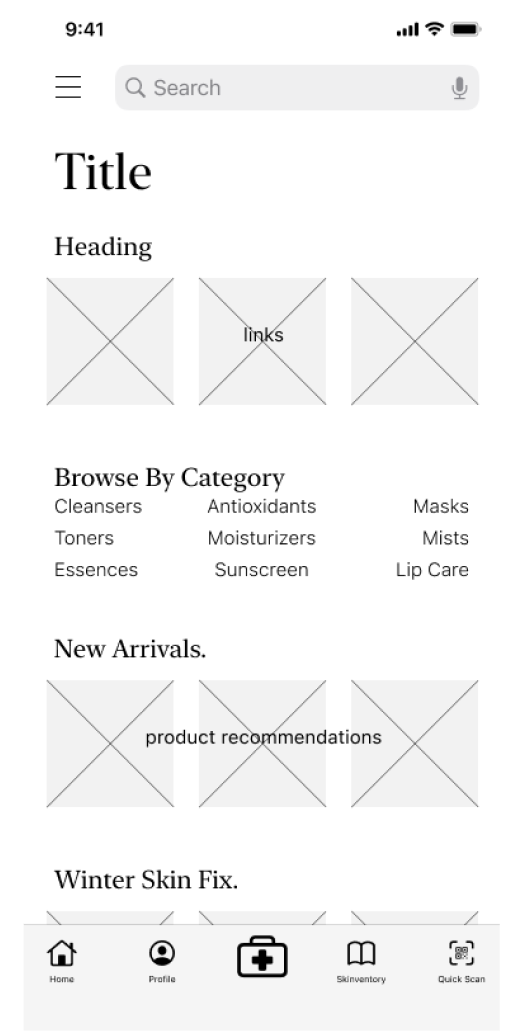
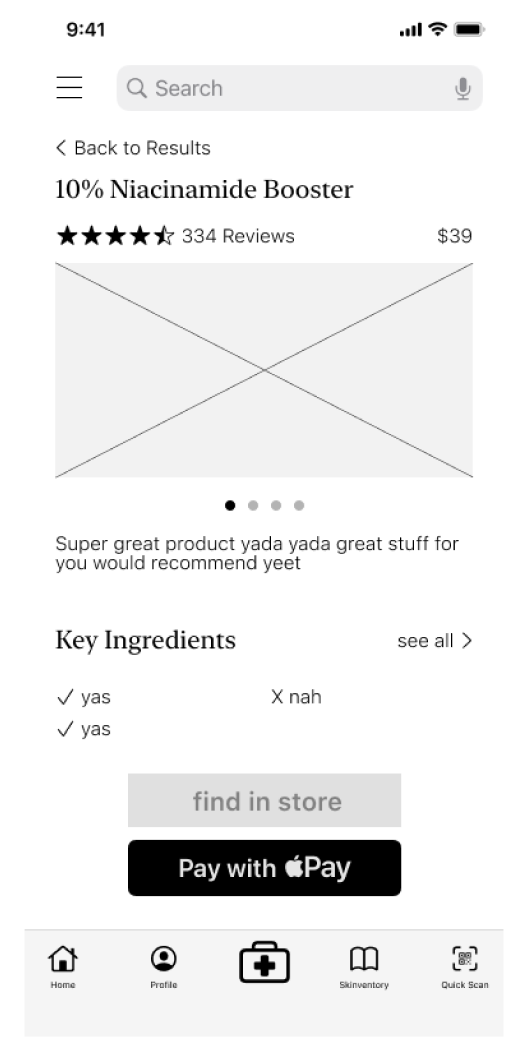
Sketches + Wireframes
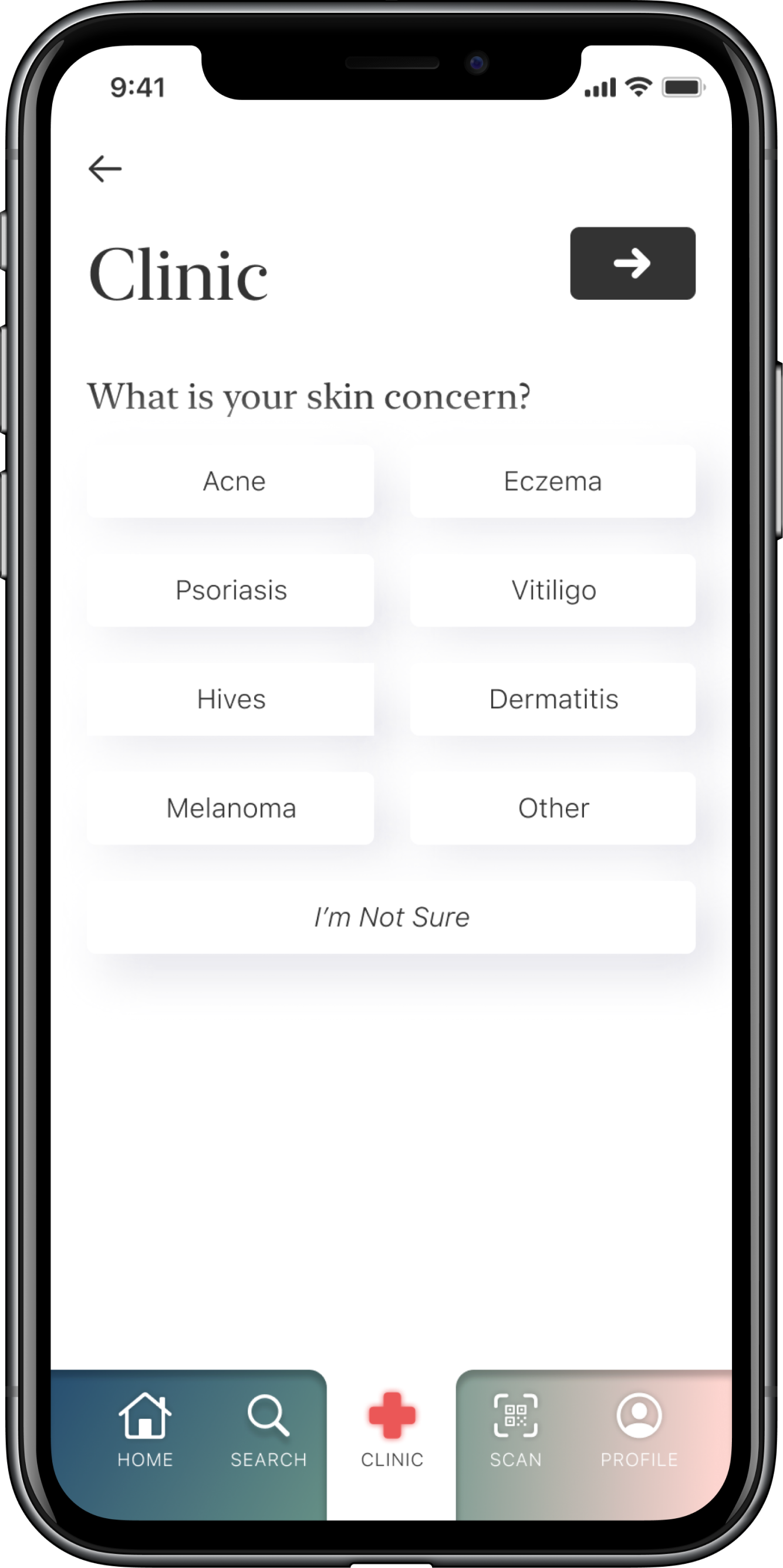
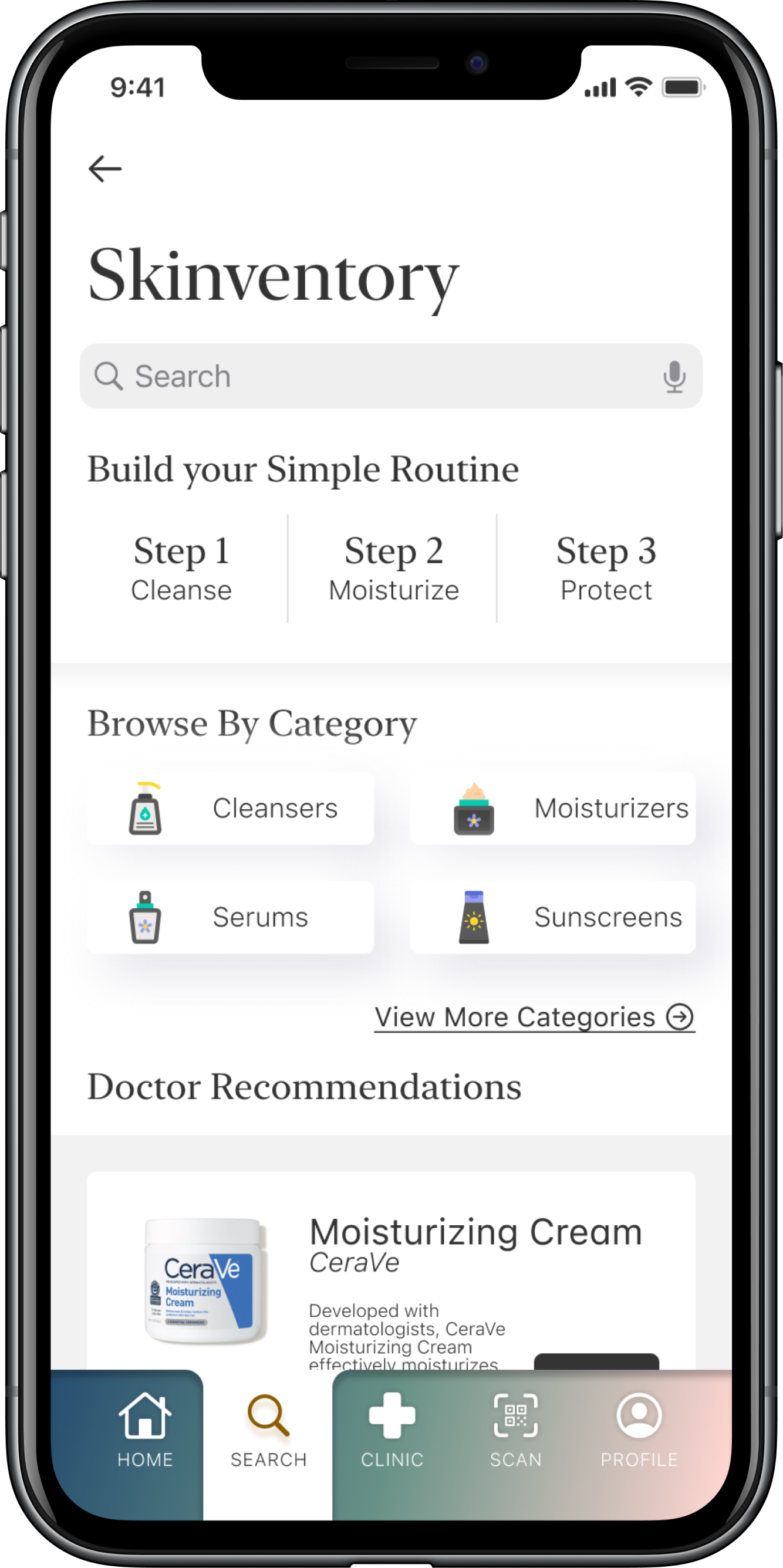
From the start, I knew I wanted two main features: a clinic to connect patients with dermatologists, and a catalog of information for users and patients alike. Opening the catalog to everyone was crucial because it allowed users from outside BC to access the great resources in it.
From the sketches, I made digital wireframes to see the concept on a digital medium. As you’ll soon find out, things changed quite quickly and quite drastically.
User Testing
I conducted two rounds of user testing, with five different participants each round. Nearly all of the participants being tested were members of the same cohort being tested over Zoom using Invision prototypes, while the remaining two were done in-person using the Invision iOS app. I kept the tasks the same throughout both rounds, which involved the following:
Log into the app
Navigate to the clinic
See the dermatologist
Search for a specific product
View product details
Here’s the results of those tests.


Some points that I found out were that the user experience seemed to be improved in the second round, as tasks were conducted quicker and with less hesitation than the previous round.
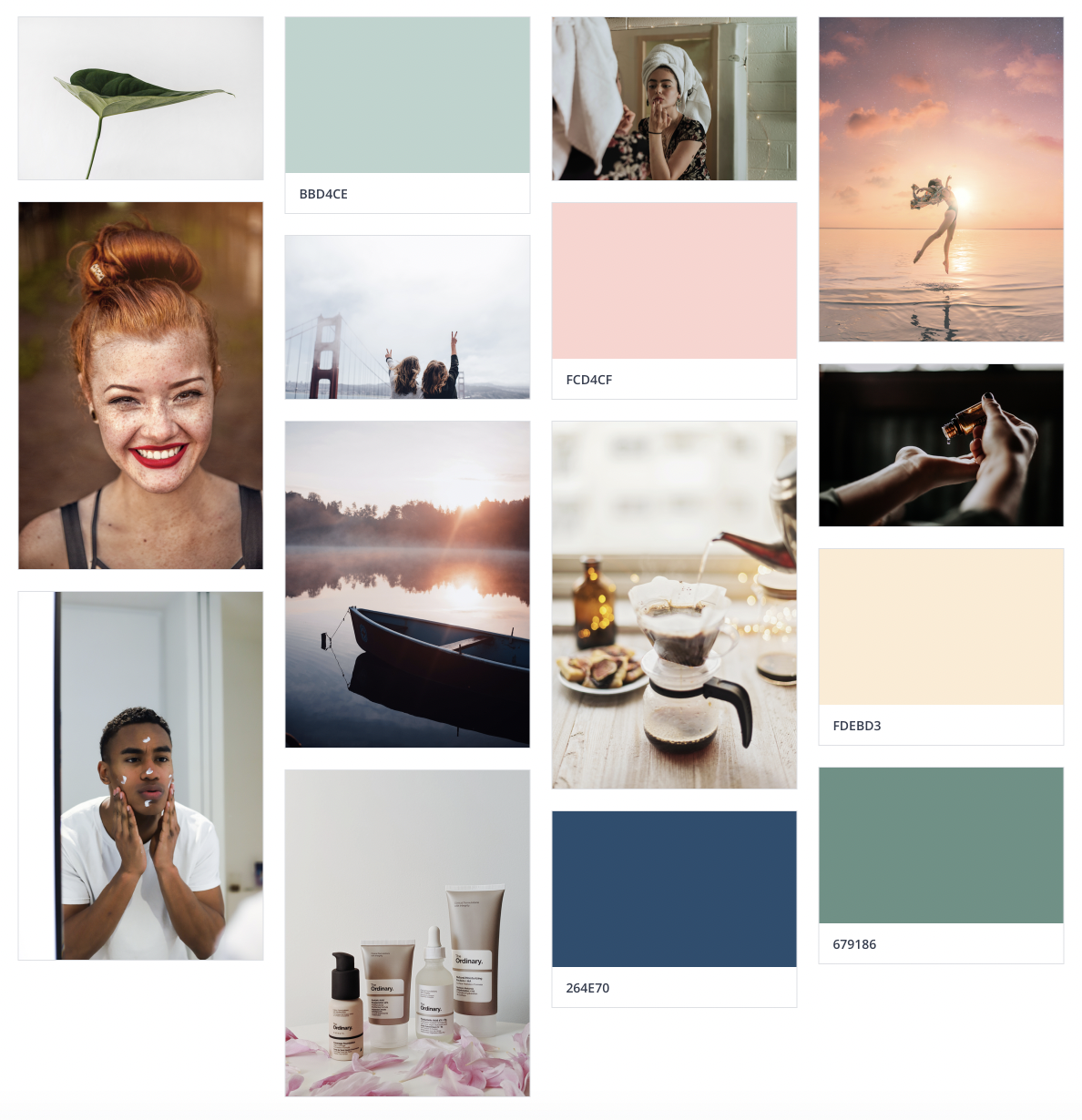
Colour + Inspiration
Iconography + Typography
Branding

Portfolio

IPS 2.0E2E Branding/Website Refresh
Illuminate the Digital LandscapeThesis Project

CliffordHospital Case Study
Autonomy in the WorkforceResearch Paper

Data WalletData Privacy Exploration

AlfreshFood Waste Sprint

DwellShopify Sprint

#OwnYourDataThesis Preparation

F(AR)MDeviancy Exploration
made with